Over the last several years, placenta encapsulation has gained increased interest. Whether it is due to a shift towards more natural ways of living or the influence of celebrities, we are happy to see women taking charge of their postpartum. Maybe you’ve heard of placenta or even wondered “should I encapsulate my placenta?” I hope this blog helps answer your questions about this process and leads you to make the best decision for yourself and your baby.
What is placenta encapsulation?

Placenta encapsulation is the process whereby your placenta is washed, steamed (or not), sliced, dehydrated and ground into powder. Your specialist will put this powder into vegetable capsules for your consumption in the weeks following the birth of your baby. Blissful Birthing provides this service in your home, and you are more than welcome to watch the magic unfold. We hope you find the following information helpful and do decide to encapsulate your placenta with us.
Will the hospital let me take it home?
In most cases, the answer is yes! Your placenta legally belongs to you and you have the right to decide what you would like to do with it after it is delivered.
Interestingly, some states consider the maternal portion to belong to the mother, and the fetal portion to belong to your baby. You can legally decide what to do with your baby’s “portion” of the placenta because your baby is a minor (which is convenient as separation would prove nearly impossible).
How can I be sure it is my placenta?
That was a concern of mine, too, before I began offering this service to clients. Blissful Birthing has the following measures and suggestions in place for your safety and peace of mind.
- You are in possession of your placenta at all times. You will not need to worry that the person coming to pick up your placenta could be in possession of multiple placentae at once. Either you or a family member will bring your placenta home ((depending if your placenta is discharged before or with you).
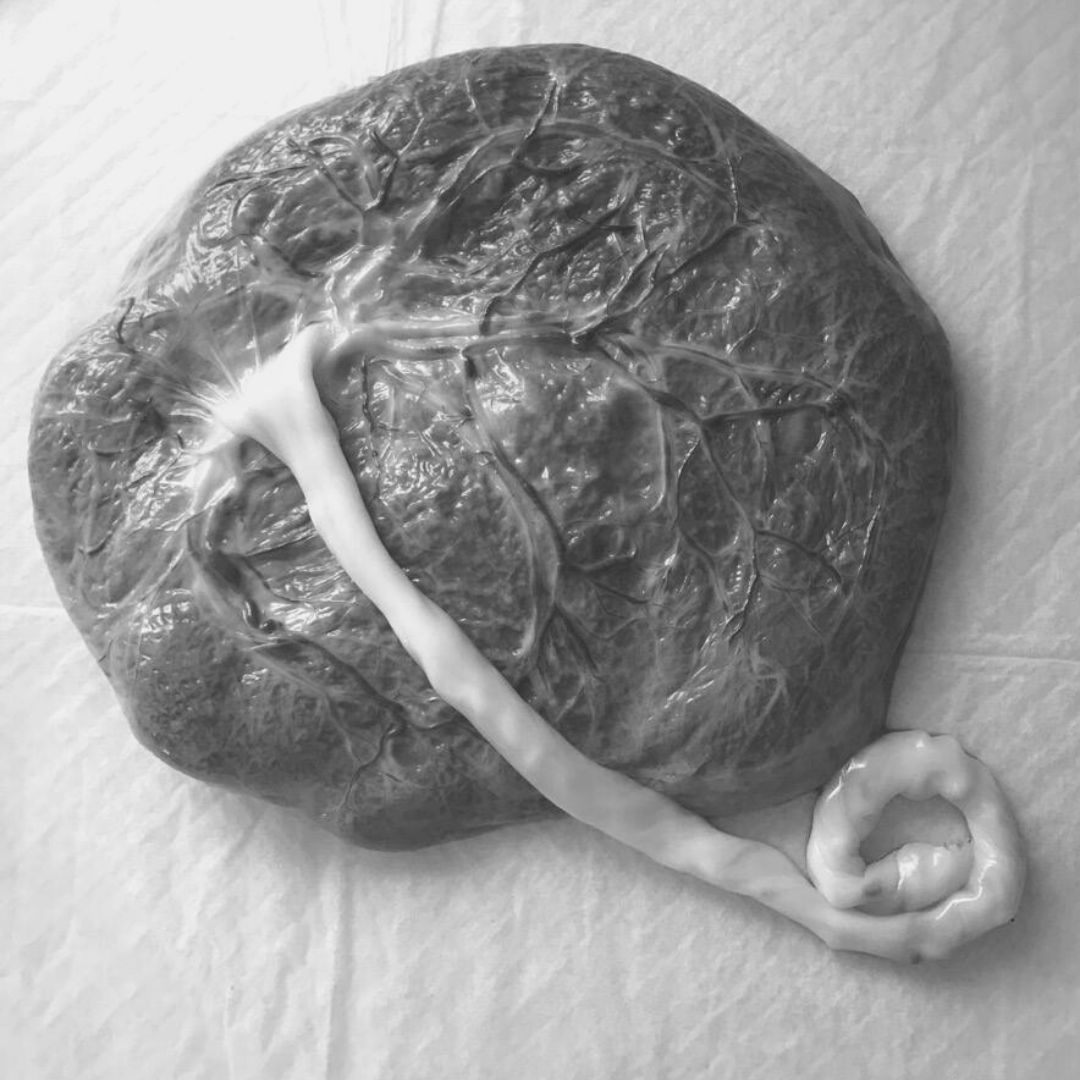
- We only process placentas in our clients’ homes, not in a dedicated workspace. If you want, you can even watch! One of my favorite aspects of providing this service is walking our clients and/or their family members through the anatomy of their placenta.
- Should your birthing location require your placenta to remain there until discharge, I would strongly suggest asking the nurse to put your medical records label on the container, and not the lid.
What are the benefits of consumption?
Our clients have reported the following benefits:
- improved mood.
- increased energy.
- replenishment of hormones.
- iron and mineral replacement.
- a more robust milk supply.
- decreased postpartum bleeding.
- less discomfort after delivery.
- lower incidence of postpartum fatigue and postpartum depression.
The FDA has not evaluated the above statements. However, preliminary research does not completely rule out these potential outcomes.
Is this practice unique to humans?
Nope! In fact, humans, camels, and marine mammals are among the exceptions in mammalian species who consume their placenta, amniotic fluid, membranes, or umbilical cord.
There are a number of theories as to why mammals engage in placentophagia, but none of them are consistently relevant among all species. Some proposed theories are:
- satisfying hunger after delivery. However, not all species decrease caloric intake before delivery.
- cleaning their nest. Many mammals are on the move soon after delivery.
- avoiding predators. This doesn’t explain why apes actually climb down the tree where they gave birth to consume their placenta (an action that puts them in danger of predation).
Can you think of other reasons why mammals may consume their placenta?
Why doesn’t everyone choose to encapsulate their placenta?
I am sure there are a number of reasons why women choose not to consume their placenta. The most common reasons I’ve heard (in a sampling from our Facebook group) include:
- thinking about it but never getting around to reserving the service.
- they heard it could decrease milk supply.
- their medical provider told them their baby could get sick.
- comfort level.
- lack of solid research.
Let’s break down some of those reasons. I cannot say that these reasons should make you choose not to encapsulate your placenta. I do not want to sway you either way. My goal is to ensure you have all the facts so you can make the best decision for yourself.
An IBCLC on the internet said it can lower my milk supply.
That blog post (linked here) explains the perspective of one lactation consultant serving families in one area. I think it is important to note that women do not seek out the help of lactation professionals if everything is going well with breastfeeding. The sample of women this IBCLC was working with already had problems with milk supply, latch, etc. Her reported sample was not representative of the population as a whole.
Her claim that she has seen a 50% decrease of milk production in her clients is concerning. But probably not for the reason you’re thinking. How did Sarah Hollister arrive at that figure? Nowhere in her post did she mention how she measured the purported drop in milk production. A claim of that proportion should, in my opinion, have some data attached to it.
Women who consume their placentas do not typically report a drop in milk production. However, if you feel your supply has dropped, reach out to your encapsulator. She can advise you on how to adjust your dose to mitigate this.
My provider told me my baby could get an infection.
The report of the mother and baby in Oregon who may have contracted GBS from placenta pills is misleading. Their provider is probably referencing this case study released from the CDC in 2017. I would urge you to give that a read and then see my comments below.
- Bacteria was cultured from samples of the placenta powder and baby’s blood, but not the mother’s breast milk. How could the bacteria get from the capsules to the baby if not through the breast milk? That’s a very good question. According to Sophia K. Johnson, et. al. “the stomach functions as a barrier against bacteria, including streptococci.” Meaning that any bacteria that was present in the capsules would be killed before the mother’s body was able to assimilate the contents of the capsule into breast milk.
- Per Boston Children’s Hospital, though rare, it is possible for a newborn to contract GBS “one week to several months” after birth. This is known as a “late onset” infection. Roughlyl 50% of babies with a late-onset infection develop it from their carrier mother. At 37 weeks, the woman in this study tested negative for GBS, but your status can change daily. It is entirely possible the mother passed the infection to her child from touching her placenta capsules and then touching her baby without washing her hands in between. That could explain how the baby and the capsules were positive for GBS but the breast milk was not.
What we do know
The placenta processor used the raw method of encapsulation (meaning the placenta was not steamed to a food-safe temperature before it was dehydrated). We know that heat above 54°C (roughly 129.2°F) can lead to a “significantly reduced number of microbiological species.” A 2018 study from Daniel Benyshek, et. al. found that “preparation technique (cooked vs uncooked) did not influence adverse neonatal outcomes.” This study looked at ~23,000 babies. It concluded that their mothers’ consumption of their encapsulated placenta put them at no increased risk for hospitalization or death than babies whose mothers did not consume their placentas. The report released by the CDC did not make mention of what temperature was used to dehydrate the placenta. We don’t know if food-safe preparation methods were used.
Keep in mind
An infection in the baby after delivery is typically indicative of the presence of an active infection during delivery. Blissful Birthing considers any signs of infection during labor and delivery (such as a fever) a contraindication to encapsulation. We also recommend washing your hands after taking your pills regardless of if you tested positive for GBS colonization. The CDC report did not mention if proper hand washing protocols were practiced.
How do you feel about these reasons and explanations? Have they changed your opinion on if you will encapsulate your placenta?
Should I encapsulate my placenta?
As you can probably see, there are many factors to consider when making this choice. I hope the information presented above, and the referenced articles provide you with a foundation for making this decision. If you answer “yes, I would like to encapsulate my placenta,” we look forward to working with you!
Please Note
The opinions mentioned above are those of Rebecca Tucci, placenta specialist, and do not constitute medical advice. The above statements have not been evaluated by the FDA. Placenta services offered by Blissful Birthing are not clinical, pharmaceutical, or intended to diagnose or treat any condition. Clients take full responsibility for their health and for choosing to use placenta encapsulation.
The following research studies were referenced in this blog:
- Human placentophagy: Effects of dehydration and steaming on hormones, metals and bacteria in placental tissue
- Placentophagy among women planning community births in the United States: Frequency, rationale, and associated neonatal outcomes
- Presence and concentration of 17 hormones in human placenta processed for cncapsulation and consumption
- Human placenta processed for encapsulation contains modest concentrations of 14 trace minerals and elements
- Hormonal Changes in the Postpartum and Implications for Postpartum Depression
- Enhancement of opioid-mediated anlagesia: A solution to the enigma of placentophagy