As many as 70-80% of women experience some morning sickness during pregnancy. Fortunately for these women the nausea and vomiting tend to subside by around 12 weeks gestation. Unfortunately, there is a small percentage of women (0.3-2% of women) who experience much more severe symptoms including nausea and vomiting, significant weight loss, malnutrition, and electrolyte disturbances. This condition is known as hyperemesis gravidarum and it can range in severity from mild (treatable with rest, dietary changes, and antacids) to severe (requiring IV fluids and nutrition).
What causes hyperemesis gravidarum?
The jury is still out on the exact causes of hyperemesis gravidarum (HG). Researchers believe it is caused by complex set of factors, including: increased hCG levels, increased estrogen levels, and pregnancy induced changes to the GI tract. Because the exact cause(s) are not known at this time, there is no way to prevent it.
Risk factors for HG may include:
- first pregnancy
- carrying a female baby
- carrying multiples
- maternal age <24 years
- obesity
- occurrence in previous pregnancies
What are the symptoms of HG?
Symptoms of hyperemesis gravidarum first appear between weeks four and six of pregnancy. Some women experience relief of these symptoms between 14 and 20 weeks, where as up to 20% of women with HG require care for the duration of their pregnancy. The following are the most common symptoms of HG:
- severe nausea and vomiting
- loss of 5% or more of pre-pregnancy weight
- decreased urination
- dehydration
- extreme fatigue
- headaches
- confusion
- jaundice
- skin changes
- low heart rate and blood pressure
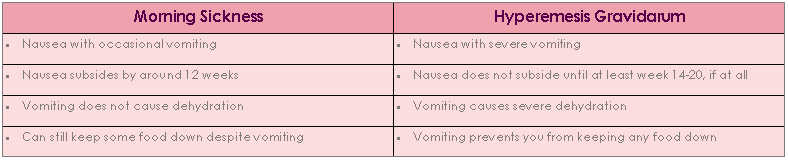
How does HG differ from morning sickness?
The following table helps to neatly outline the main differences between morning sickness and HG.
How is hyperemesis gravidarum diagnosed?
Only your doctor can diagnose HG. They will want to rule out: GI problems, thyroid problems, liver problems, and neurological disorders. Then they will look at your weight loss, blood and urine levels (to check for signs of dehydration, electrolyte imbalances, and the presence of ketones), and assess your overall condition.
What treatment options are there?
Because hyperemesis gravidarum is a complex condition with unknown causes it can be difficult to treat. Your doctor’s highest priority is to prevent and correct any nutritional deficiencies you may be experiencing, promoting a healthy outcome for you and your baby. Treatment will depend on your past medical history and you current lab values, but may include the use of IV fluids, antiemetics (antinausea drugs) and dietary supplements. Your doctor may also suggest dietary changes, including: avoiding fatty foods, not eating and drinking at the same time (drink between meals, not with them), eating slowly, not laying down for at least 2 hours after eating, avoiding spicy/flavorful/aromatic foods, and eating very small amounts frequently. If you are interested in reading the complete findings published in the Reviews in Obstetrics and Gynecology, it can be found here.
Only a doctor can diagnose and prescribe treatment for hyperemesis gravidarum. If you suspect you have HG, we encourage you to seek treatment with your medical team as soon as possible. This blog post is for informational purposes only.
Additional Blogs in This Series
I is for Induction
J is for Jaundice
K is for Ketosis
This blog is for informational purposes only. It does not take the place of consultation with your healthcare professional