Epidural anesthesia is the most common form of pain relief during labor and delivery. An epidural is a medical procedure whereby a catheter is inserted into the epidural space of your spinal cord and medication is injected. You will become numb below the placement site. Medication is administered via this catheter until after you deliver your baby.
What can I expect?
Before the anesthesiologist can place your epidural you must receive at least one liter of fluids via IV. This because an epidural can cause a drop in blood pressure. To combat this, your blood volume will be increased with IV fluids. The nurse will continue to hang fluids throughout the remainder of your labor. After receiving fluids, the anesthesiologist will come in and go over the procedure and obtain consent.
 You will then be instructed to sit with your legs off the side of the bed and curl over, opening up the space between your vertebrae. The anesthesiologist will locate the place where the epidural will be placed (between the L4 and L5 vertebrae) and mark the area.
You will then be instructed to sit with your legs off the side of the bed and curl over, opening up the space between your vertebrae. The anesthesiologist will locate the place where the epidural will be placed (between the L4 and L5 vertebrae) and mark the area. 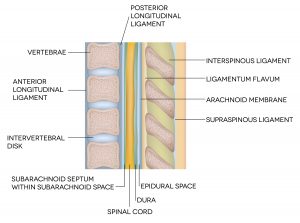 This location will be swabbed three times in an outward circular motion and then covered with a sterile drape. A local anesthetic will be given where the epidural will be placed. This will feel like a prick and stinging and should be the only part of the epidural placement that you feel pain. Once the local anesthetic has taken effect, a longer needle will be inserted into the epidural space of your spine.
This location will be swabbed three times in an outward circular motion and then covered with a sterile drape. A local anesthetic will be given where the epidural will be placed. This will feel like a prick and stinging and should be the only part of the epidural placement that you feel pain. Once the local anesthetic has taken effect, a longer needle will be inserted into the epidural space of your spine.
To orient you, the accompanying image shows your spinal column on the left. This needle is hollow and allows the anesthesiologist to guide the epidural catheter into place, where the medication will be delivered. The most common drugs used for epidural anesthesia are ropivacaine and fentanyl. You will then lay on your back for 20-30 minutes while the drugs spread and take effect. Lying flat helps to ensure that the pain medication distributes more evenly between both of your legs. The anesthesiologist will make sure you are numb before setting you up with a continuous drip of pain medication.
Are all epidurals the same?
You may have heard of a “walking epidural.” We have not found an anesthesiologist in our service area who will place an epidural and then give you the green light to walk around. The risk of your blood pressure dropping combined with the lack of sensation in your legs is too much of a liability. However, we have noticed that the anesthesiologists are leaning towards providing a lower dose of medication so you can move around in the bed (with help) and still feel pressure (but not pain).
It is also not uncommon for your provider to stop or turn down the epidural medication as you get closer to pushing. Why, you ask? Well, if you are completely numb you won’t feel anything and it is less likely that you will be able to effectively push. Decreasing the dose of medication will allow you to feel pressure, if you aren’t already, but still keep the pain at bay, and may allow you to maneuver into a position other than your back to push.
When should I get my epidural?
You can get an epidural at any time once labor has begun. The longer you wait to get an epidural, the less likely it will be that you may need other interventions. For this reason we recommend waiting until you are 7-8 cm dilated, if you can and want to, before requesting an epidural, if that is part of your birth plan. However, everyone has different levels of pain tolerance and this is your birth and your decision to make. Our doulas are trained to support clients who get epidurals. Let’s look at why getting an epidural earlier in labor may increase your chances of other interventions.
 Once the epidural is placed you must stay in bed, so you aren’t able to encourage your baby to move down using gravity or methods that can widen your pelvic outlet (bouncing on a ball, squats, double hip squeeze, etc). Because you are laying down the ability of your baby to make meaningful, or effective, contact with your cervix can be reduced. Your doula can help you get on your side and use either a peanut ball or pillows to open your pelvic outlet, helping to make your contractions more effective.
Once the epidural is placed you must stay in bed, so you aren’t able to encourage your baby to move down using gravity or methods that can widen your pelvic outlet (bouncing on a ball, squats, double hip squeeze, etc). Because you are laying down the ability of your baby to make meaningful, or effective, contact with your cervix can be reduced. Your doula can help you get on your side and use either a peanut ball or pillows to open your pelvic outlet, helping to make your contractions more effective.
Epidurals block some of the oxytocin receptors in your uterus, which can cause a change in contractions (either in their strength, frequency, or both). Your provider may suggest the placement of an intrauterine pressure catheter to measure the strength of your contractions. They will insert this flexible wand into your uterus between your uterine wall and your baby.
You will receive fluids during your labor and will not be able to get out of bed. It is very likely that a catheter will be placed in your bladder until it is time to push. If your bladder is full, it can hinder your uterus’ ability to fully contract.
What are the risks?
As you know by now, we are non-medical birth professionals. You can call the anesthesia department where you will deliver and discuss risks and benefits with an anesthesiologist. Having this conversation before you are in labor will help you make a truly informed decision.
To briefly outline some of the risks, they may include:
- longer labor
- failure of labor to progress
- longer second stage of labor (pushing)
- increased need for instrument assisted delivery (forceps or vacuum)
- increased risk of vaginal tears
- incomplete or uneven numbing
- spinal headache
- paralysis
- tingling in the legs
- back pain after delivery
- fever (as a foreign object inserted into the spinal cord triggers an immune response)
- difficulty with breastfeeding (because the epidural blocks oxytocin, which is essential for your milk to come in)
However, epidurals are effective at relieving pain and epidurals can be helpful. If your labor is long, getting an epidural can help you to get the rest you need to keep going. The medication in the epidural relaxes your pelvic muscles. Relaxed muscles can help make it easier for your baby to move through the birth canal, helping you avoid a C section in some cases.
There is no right or wrong decision when it comes to using an epidural for pain relief during your labor. Speak with your provider or a member of the anesthesia department to decide if an epidural is right for you.
If you liked this blog, you may also like:
F is for Formula
G is for Group B Strep
H is for Hyperemesis Gravidarum
This article is for informational purposes only. The information here does not replace consultation with your healthcare professional. Speak with your doctor before making any and all medical decisions.