“Induction” is any of a number of artificial methods, both medical and non-medical, for bringing on the start of labor. According to the CDC the induction rate in the United States is around 23.3%. Reasons for induction can range from convenience or wanting to pick your baby’s birthday (elective inductions) to the prevention or remediation of life threatening complications (medically necessary inductions). By the end of this post you will understand:
- what induction is
- why you may be induced
- alternatives, risks, and outcomes
- common misconceptions.
When would my provider induce labor?
As mentioned, there are many reasons for induction of labor.
- Post-Due (at or beyond 42 weeks). If there are no signs of labor and you are past your due date, your provider may suggest induction. While there are great variations in “full-term” pregnancies, there comes a time where your provider becomes increasingly concerned about your baby passing meconium, the integrity of your placenta, and the risk of stillbirth.
- Complications. These complications may include: preeclampsia, low or high fluid levels, compromised blood flow to the placenta or baby, gestational diabetes, concerns about placental integrity.
- Rupture of Membranes with no Contractions. Every provider and birthing facility is different in how long they are comfortable letting you wait for labor to progress one your water has broken. After 24 hours the vast majority of providers will want to perform a C section because of the increased risk of infection. If your labor has not begun to progress on its own, your provider may try to induce labor to start before you reach the 24 hour mark.
- Elective Reasons. If your previous labor was very fast and you are concerned about getting to the hospital on time, your work schedule requires you to be back in the office by a certain date, or your partner has work commitments, you may be able to be electively induced. Providers try to avoid induction before 39 weeks because babies’ lungs are not fully mature (and they want to reduce the chance of a visit to the special care nursery). Elective inductions are at the discretion of your medical provider.
Is a C Section Ever Preferable?
It may be! Some providers feel a C section is a safer choice for both mom and baby if:
- either of you are in distress
- the baby is not descending in the birth canal
- the umbilical cord is prolapsed
- baby is breech
- there are complications with the pregnancy
- you are post-due and not showing signs of labor
- your placenta is partially or fully covering your cervix (placenta previa)
- you have an active genital herpes outbreak
A C section in and of itself is not “bad”. For this reason we suggest speaking with your provider about the risks and benefits of a C section vs induction.
How does it work?
I feel like I’m starting to sound like a broken record, but every provider and birthing facility are different in the methods they use for inductions. The following methods are the most common. Your provider may opt for one or a combination of any of them depending on you, your baby, and the circumstances surrounding your induction.
- Cervical Ripening. Needed if the cervix shows no sign of dilation or effacement. A prostaglandin gel or suppository can accomplish this. The prostaglandins soften your cervix and promote dilation and effacement. If you have already begun to dilate, your provider may use a Foley Bulb, a catheter with a balloon on the end of it, to manually dilate your cervix to 4 cm.
- Stripping/Sweeping of Membranes.Your provider can strip your membranes if the amniotic sac is intact and you are dilated. They will insert a finger into your uterus and move it between the sac and uterine wall. This may release prostaglandins, promoting uterine contractions and cervical dilation.
- Artificial Rupture of Membranes. This is an unintended consequence of stripping your membranes or done intentionally once labor has begun. Artificial rupture of membranes (AROM) involves breaking your waters manually with an instrument that looks like a crochet hook. AROM helps labor progress by allowing your baby’s head to make stronger and more meaningful contact with your cervix during contractions.
- Pitocin. A synthetic form of oxytocin, the hormone of labor and delivery, breastfeeding, and bonding. Your doctor will order pitocin to be given slowly via IV. Pitocin will induce or augment your contractions. Expect a marked increase in the strength, regularity, and frequency of contractions within 30 minutes of the IV beginning.
What are some alternatives to a medical induction?
Glad you asked! We have a blog post on Natural Ways to Induce Labor. Without going into the detail of that post, I will list some non-medical options for labor induction below.
Discus even non-medical methods of induction with your OB/GYN or midwife. Your provider best knows your medical history and what your body and your baby can safely tolerate.
- Sex (with ejaculation in your vagina)
- Nipple Stimulation
- Walking, especially on uneven surfaces
- Lunges or Squatting on a birthing ball
- Spicy food (or any food that causes you to have loose bowel movements)
- prostaglandins cause loose bowel movements. They also promote cervical ripening.
Risks, Outcomes, and The Cascade of Interventions
A 2005 study by the American College of Obstetricians and Gynecologists found that inducting first time moms was directly associated with an increased risk for Cesarean delivery. 23.8% of elective inductions and 23.4% of medically necessary inductions ended in a C section compared with 12% of women who go into labor spontaneously.
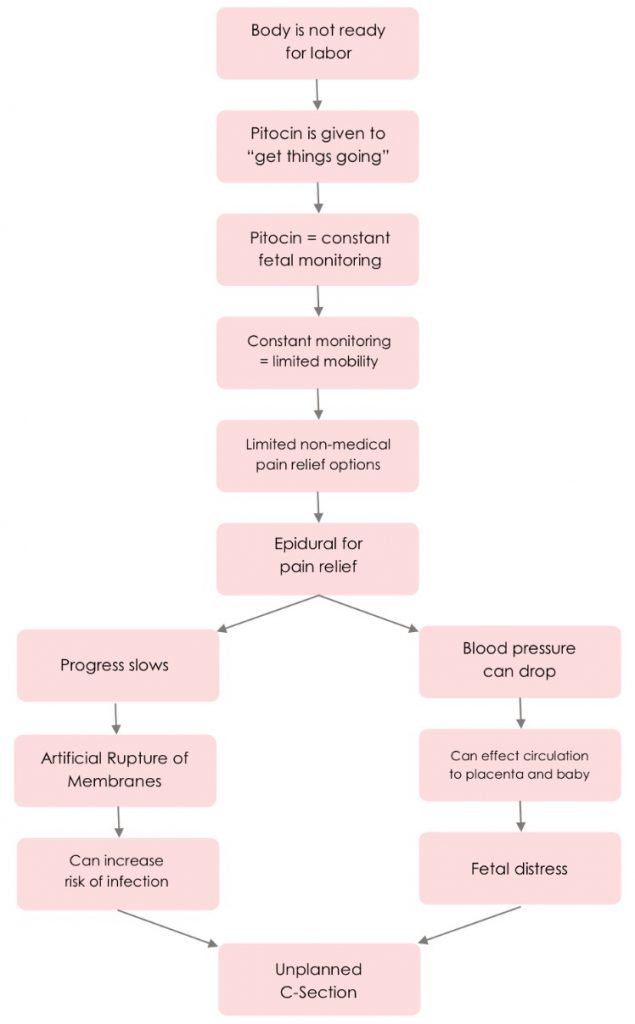
One phrase that frequently comes to mind when pregnant women hear “induction” is Cascade of Interventions. An induction does not necessarily mean you will experience this cascade of interventions or that you will need a C section.
Induction ≠ Cascade of Interventions.
However, additional interventions (such as those outlined in the accompanying diagram) can become more likely. Speak with your OB/GYN or midwife with your questions and concerns regarding induction.
Common Misconceptions
Many of our clients are anxious about inductions because they do not want a high-intervention birth. You can still have a low-intervention delivery that did not begin spontaneously.
You are more likely to have a vaginal delivery with an induction if you have a favorable Bishop Score and your baby is positioned properly.
Delivery without an epidural is possible if you have been induced! Yes, many women report their contractions being more uncomfortable with pitocin, but that does not mean you’ll require an epidural. Our doulas are experts at instilling strength and dispelling fear by providing our clients physical, emotional, and informational support during pregnancy and labor and delivery.
FREE Printable Worksheet
We have created this worksheet for you to use if your medical provider has brought up an induction of labor. It can help you start a conversation with your provider so you better understand what they are proposing and decide if this is the best choice for you and your baby. You can access the worksheet here.
More Blogs in This Series
J is for Jaundice
K is for Ketosis
L is for Lochia
This blog is for informational purposes only. It does not take the place of consultation with your healthcare professional.

Comments 2
Pingback: O is for Oxytocin | Blissful Birthing
Pingback: F is for Formula | ABC Blog Series | Blissful Birthing